- Centers & Services
- Birthing Services
- Cardiovascular Services
- Cardio-Pulmonary Services
- Diagnostic Imaging – Radiology
- Emergency Department
- Health Partners of New Site
- Hospital Medicine
- ICU/Step-Down Unit
- Laboratory
- Mammography – Women’s Center
- Medical Park Family Care
- OB-GYN Associates at Russell Medical
- Pediatrics
- Pharmacy
- Russell Medical Orthopaedics & Sports Medicine
- Russell Retail Pharmacy
- Sleep Disorders Center
- Surgical Services
- Total Fitness Physical Therapy
- Total Healthcare
- Transitional Care Unit
- Urgent Care
- Wound Care and Hyperbaric Medicine
- UAB Medicine at Russell Medical
News & Events

Home / News & Events
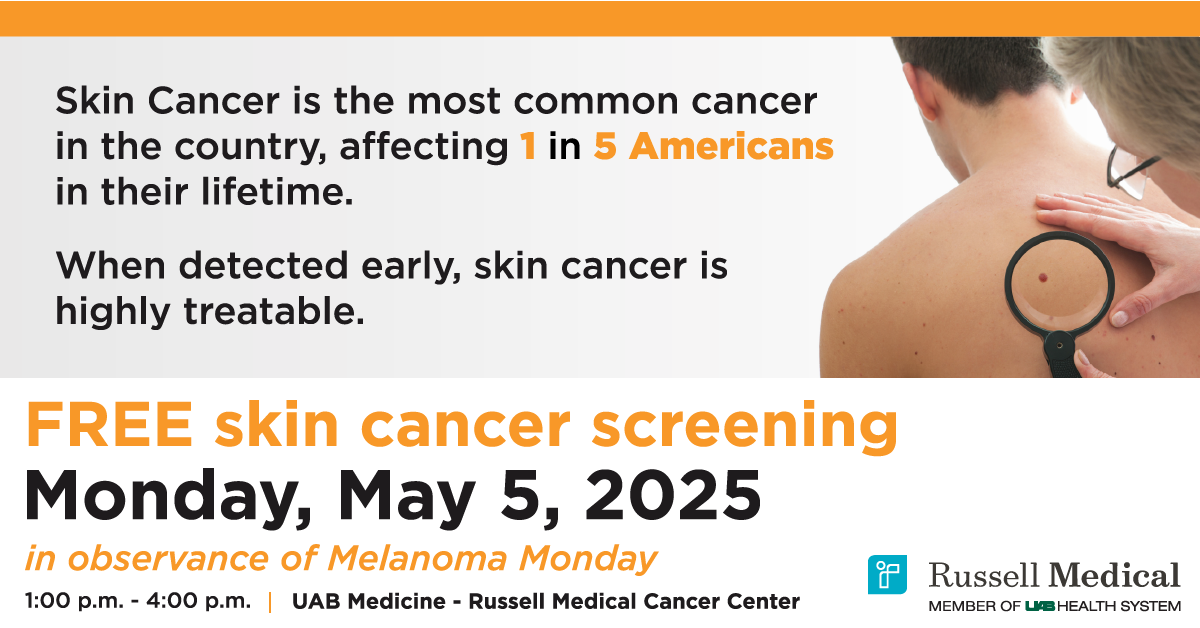
FREE Skin Screenings by board-certified dermatologist, Dr. Steven Mackey on Monday, May 5th, 2025
1-4 p.m. at UAB Medicine – Russell Medical Cancer Center
No Appointment necessary!
Operation Wipe Out Cervical Cancer
Cancer Thrivers Support Group
-
- Meets the first Tuesday of every month at 5:00 p.m. in the Cancer Center Conference Room

News & Events:
Rosa Robot
Benjamin Russell Legacy Project
Community Health Video Series
Price Transparency
Russell Retail Pharmacy
News You Can Use
#5759 (no title)
1557 Non-Discrimination Disclosure
Cancer Resources
Careers
Centers & Services
CEO Announcement
Contact
Donate
EMTALA Disclosure
General Information
Gift Shop (Info)
Heart Screenings
Hospital Week
Important Medicare Information for Russell Medical Patients
Job Application
Notice
OB-GYN Associates at Russell Medical
Patients
Providers
Special Accommodations
Tutu 2.2 Fun Run
Tutu 2.2 Fun Run for Breast Cancer Awareness
UAB Medicine at Russell Medical
Urgent Care
Visitors